- 作者/章振旺醫師
- 本文轉載自 Care Online 照護線上《超糗!開會狂跑廁所十幾次 竟是潰瘍性結腸炎》,歡迎喜歡這篇文章的朋友訂閱支持 Care Online 喔
「醫師,我上班狂跑廁所,一天拉十幾次,真的很困擾!尤其遇到公司開會,我就更緊張,因為肚子不聽使喚,必須頻繁進出會議室廁所折返跑,嚴重影響工作效率跟同事觀感。這樣的腸胃症狀時好時壞持續一年多,原以為是腸躁症,自行到藥局拿藥吃,但是近來發現症狀加劇,還伴隨血便、頭暈、疲倦等症狀,這才驚覺不對勁來就醫。」三十多歲的邱先生一臉憂慮地問。
「你的狀況恐怕不單純是腸躁症,我們趕快安排抽血並大腸鏡檢查,以利及早確診治療。」馬偕紀念醫院胃腸肝膽科章振旺醫師回憶這起個案,當時藉大腸鏡檢查,發現患者的腸子黏膜有大片表淺潰瘍及許多細小糜爛斑,同時根據患者病史及臨床表現,診斷為潰瘍性結腸炎。
潰瘍性結腸炎不易覺察,三成患者耗時兩至三年確診
章振旺醫師表示,約有三成潰瘍性結腸炎患者,平均就診超過五位以上醫師、歷經二到三年才能確診,期間往往讓患者身心俱疲。醫師指出,潰瘍性結腸炎臨床上診斷不易,症狀表現容易與腸胃炎及腸躁症混淆,無法透過單一指標確診,必須根據患者病史、抽血檢驗、大腸鏡檢並搭配病理切片等資訊綜合評估。
此疾病常見症狀為腹瀉、腹痛、疲倦、食慾不振、發燒,當大腸黏膜發炎潰爛嚴重時,可能解出血便、黏液便。一但血便持續發生,恐導致貧血、頭暈。章振旺醫師提醒,潰瘍性結腸炎好發於年輕人,以學生、上班族居多,疾病症狀對課業、工作影響甚劇,尤其疾病發作,患者還得向公司、學校告假,甚至住院接受治療。
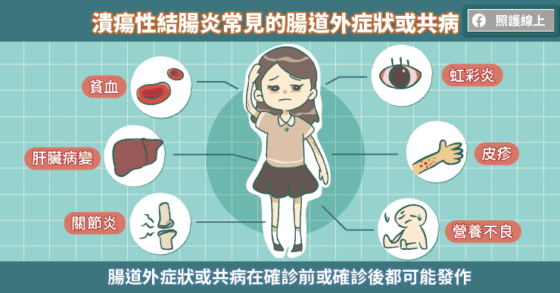
章振旺醫師指出,潰瘍性結腸炎屬於慢性自體免疫疾病,正常狀況下,我們的免疫系統只會攻擊侵入體內的外來物,但是當免疫系統出狀況時,對體內組織發動攻擊,導致慢性發炎。潰瘍性結腸炎就是一例,除了侵犯腸道外,還可能伴隨腸道外症狀,如皮疹、虹彩炎、肝臟病變、關節炎等,等於全身都受到影響。
在台灣,至少有一成患者伴隨有腸道外症狀,但根據國外研究可能高達四成,其中最常見的是關節炎。潰瘍性結腸炎的腸道外症狀有四分之三在診斷後才發現,但仍有四分之一在被診斷前就有腸道外症狀。除了腸道外症狀外,潰瘍性結腸炎還可能有併發症或共病的產生,如貧血、營養不良、腸穿孔……等,罹病時間越久,產生的機會就愈高。
早期治療控病情,降低併發症風險
該名個案邱先生確診後,先後接受口服藥、塞劑及短期類固醇治療,症狀一度緩解,但幾個月後,血便症狀再現,在使用免疫調節劑後,因為發生副作用只得暫時停藥。後續追蹤發現腸道發炎狀況加劇,因此,隨即申請生物製劑治療,所幸使用生物製劑後,臨床症狀好轉,患者黏膜發炎的狀況明顯改善,也解決他上班時得經常跑廁所的窘境,生活及工作品質獲得改善。
章振旺醫師解釋,在 1970 年代,5-ASA 抗發炎藥物被使用於治療潰瘍性結腸炎,而後具有抑制免疫功能的類固醇開始廣泛用於急性期患者,但不建議長期經常性使用。時至 1990 年代,免疫抑制劑漸漸成為治療選項,醫師根據患者病情嚴重度,給予不同治療組合。 若上述傳統治療效果不佳,會進一步考慮使用生物製劑。
近年來,隨著生物製劑發展,潰瘍性結腸炎的治療成效相對提升。目前的治療目標不只是緩解症狀,而是持續治療使腸道黏膜癒合。根據病患治療反應調整,持續治療能控制疾病,減少住院的機會。
除了藥物治療外,如腸道持續嚴重發炎導致穿孔或出現毒性巨結腸等嚴重併發症時,患者就得需要外科介入,接受手術切除部分腸道。若能早期接受治療、控制病情,有助減少反覆手術的機會。
腸保健康有 3 要:用藥、飲食、作息要注意
潰瘍性結腸炎雖無法治癒但可以控制,提醒患者腸保健康有三要,一要遵照醫囑,切勿自行中斷停藥;二要飲食也需掌握定時定量、避免刺激性、增加腸胃負擔的食物等原則,患者平時也可自我觀察,若吃了某些食物會出現不適時,可與醫師與營養師討論,未來盡量避免食用,降低不適發生;三要維持正常作息、避免熬夜、並養成規律運動的習慣,因為健康的生活型態有助維持免疫系統穩定。

章振旺醫師指出,潰瘍性結腸炎急性發作時,患者的治療配合度較高,不過症狀一但緩解,很容易掉以輕心,未能按時服藥,甚至擅自停藥,如此一來,容易讓病情復發,也更難控制。
醫師提醒,即使症狀緩解、沒有不適,也應持續治療、定期追蹤,才能穩定病況,與潰瘍性結腸炎和平共存!
- 本文轉載自 Care Online 照護線上《超糗!開會狂跑廁所十幾次 竟是潰瘍性結腸炎》,歡迎喜歡這篇文章的朋友訂閱支持 Care Online 喔
- 加入照護線上 LINE 官方帳號,健康資訊不漏接!